Started more than a decade ago, digital transformation in Healthcare was slowed down by the worldwide pandemic and still has obstacles to moving further. One of them is legacy software that healthcare providers widely use. Even though there are valid reasons for that, for example, deep integration into processes or patients' info storing and safety concerns, they most likely become a part of uncomfortable, slow, and bureaucratic services.
Legacy healthcare systems usually include electronic health record (EHR) systems, payment and administration platforms, medical devices, and communication networks. This software has not been updated in a long time (or cannot be updated anymore), making it difficult to adapt to regulatory requirements, clinical workflows, and patient needs.
Healthcare legacy systems modernization allows you to solve several issues at once, from enhancing patient care to improving operational efficiency. It helps you to automate most processes, speed up data processing, integrate with third-party applications and devices, implement new disruptive features, improve service, and, as a result, care for patients.
According to KMPG Healthcare and Life Science Investment Outlook 2024, more than half of healthcare providers that took part in the survey named EHRs and virtual health, such as telemedicine and remote monitoring, among the most attractive areas for investment in 2024. Also, 4 in 10 ranked clinical workflow solutions and population health management among the most appealing.
However, the need for change does not equal the ease of its implementation. On the way to upgrading healthcare providers can face some serious challenges: too complicated infrastructure that requires vast time and budget investments, data migration and security issues, regulatory compliance, and more.
Scale your business effortlessly with modernized IT solutions
In this article, we'll take a detailed look at the potential risks and benefits of upgrading Healthcare Legacy systems and provide tips on making the transition as safe and budget-friendly as possible.
Understanding Legacy Systems in Healthcare
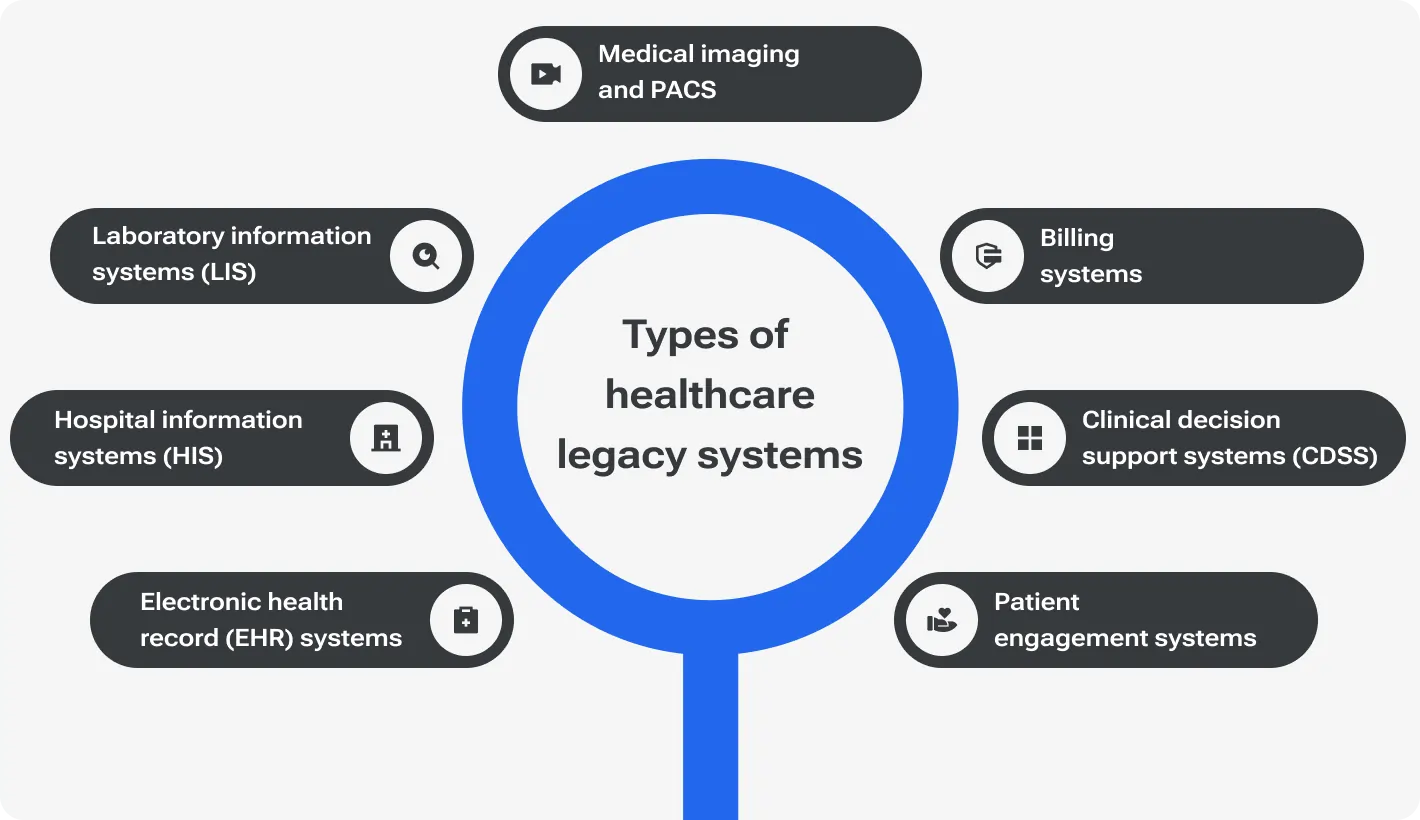
First things first. Before proceeding to legacy healthcare solutions, let’s find out what is a legacy system in healthcare and why we should modernize it. In general, healthcare legacy systems refer to any outdated software that is still in use, however, there are several most common types with particular issues to solve.
Types of Legacy Systems Commonly Found In Healthcare
Legacy EHR systems are extremely crucial for most hospitals and healthcare providers, however, they lack compatibility with external systems, which leads to fragmentation of patient data across healthcare facilities. Moreover, legacy EHRs usually have limited support for mobile access, making it difficult to access patient information on the go.
Remember those hours of waiting for employees to find essential data or wait for results from other departments? This is all because of the legacy HIS. Most often, their problem lies in outdated data storage and exchange technology, which reduces efficiency and slows down all data management processes. Legacy HIS systems do not scale well and cannot keep up with the ever-growing needs of the medical field.
LIS digitization made it possible to quickly place a request and receive test results, store and manage them. However, this system still requires regular updates to comply with constantly emerging new testing technologies, as well as data standardization.
The most common problems with legacy PACS are limited memory storage and slow performance. In addition, due to a lack of updates or outdated hardware, they are difficult to integrate with modern systems that may not accept the format or size of images.
Medical billing in general is quite a sensitive and stressful topic for patients, and errors that occur due to the use of outdated systems add to the stress. Legacy billing systems usually operate on too old code or use manual data entry that leads to system crashes or billing errors.
What should help make a more informed decision can actually delay it or, on the contrary, give harmful advice. Limited integration with EHRs and a lack of real-time data lead to reduced effectiveness in providing timely and evidence-based recommendations.
These systems are designed to improve the interaction between the patient and the healthcare provider. However, their implementation from the very beginning did not take into account the need for interactive functions and a user-friendly interface, which is currently the main obstacle to using the systems at their maximum effectiveness.
All these systems usually make up a large and rather comprehensive architecture of legacy software, which makes it difficult to modernize it in simple and easy ways. Nevertheless, you should understand that using healthcare legacy systems leads to a decrease in institution efficiency and income, a downturn in patient care.
How Do Outdated Systems Impact Healthcare Outcomes?
As the name implies, Healthcare primarily cares about patients, this is where the first problems of using outdated software appear.
Legacy healthcare systems are quite slow and poorly scalable. It means the employee will have to spend a lot of time looking for necessary information or waiting for lab results to come. Medical treatment is a sphere where time is crucial. The lack of real-time information may cause misdiagnosis or delays in critical medicine for patients. Well, actually, this is the worst-case scenario but using outdated software leads to many errors, delays, and unpleasant situations in the process of providing care to patients.
Insufficient flexibility or the lack of it does not allow legacy software to integrate with the latest technology or to expand with new options. Moreover, the multitude of problems with storing information and obtaining access to it leads to a slowdown not only in the work of personnel but also in data processing. There is no quick and proper communication between departments, and it requires additional effort. The efficiency and productivity of work is significantly reduced due to the use of outdated software, which leads to a decrease in the number of patients who can be helped.
Moreover, the cybersecurity of using outdated equipment is also a big question. Because sensitive and confidential patient information, financial data and other info that must be stored and encrypted with reliable modern protocols are at risk. The regulatory policy of most international healthcare organizations requires medical organizations' software to comply with international standards. Violation of this rule can entail serious reputational and financial losses.
So, it is obvious that healthcare legacy systems modernization is one of the ways to overcome these crucial issues.
The Case for Modernization
Surely, at this point, you understand the importance of legacy modernization. But how to identify, if you already need it?
Here is a checklist “How to know when it's time to upgrade your healthcare software”:
Limited functionality:
Documents types or data formats are limited;
You can't easily integrate with the newest techs;
You can't implement new options due to difficulty or technology outdated;
Your OS environment is no longer supported by the provider;
Automation for routine tasks is impossible or very limited;
You still depend on hardware characteristics that must be compatible with your system.
Frequent malfunctions:
Software crashes and replicates glitches;
Apps operate too slowly even with basic inquiries;
Poor performance of the software affects staff and the quality of their services;
Constant delays and errors lead to unsatisfied patients;
Usual reports and information are hard to input and form;
The system constantly fails performance tests.
Another thing to consider is when your Healthcare product is no longer supported or abandoned by its vendor. Sometimes vendors offer newer versions of their product or other more efficient solutions that replace the previous one. In this case, you use third-party legacy software that should be upgraded or replaced.
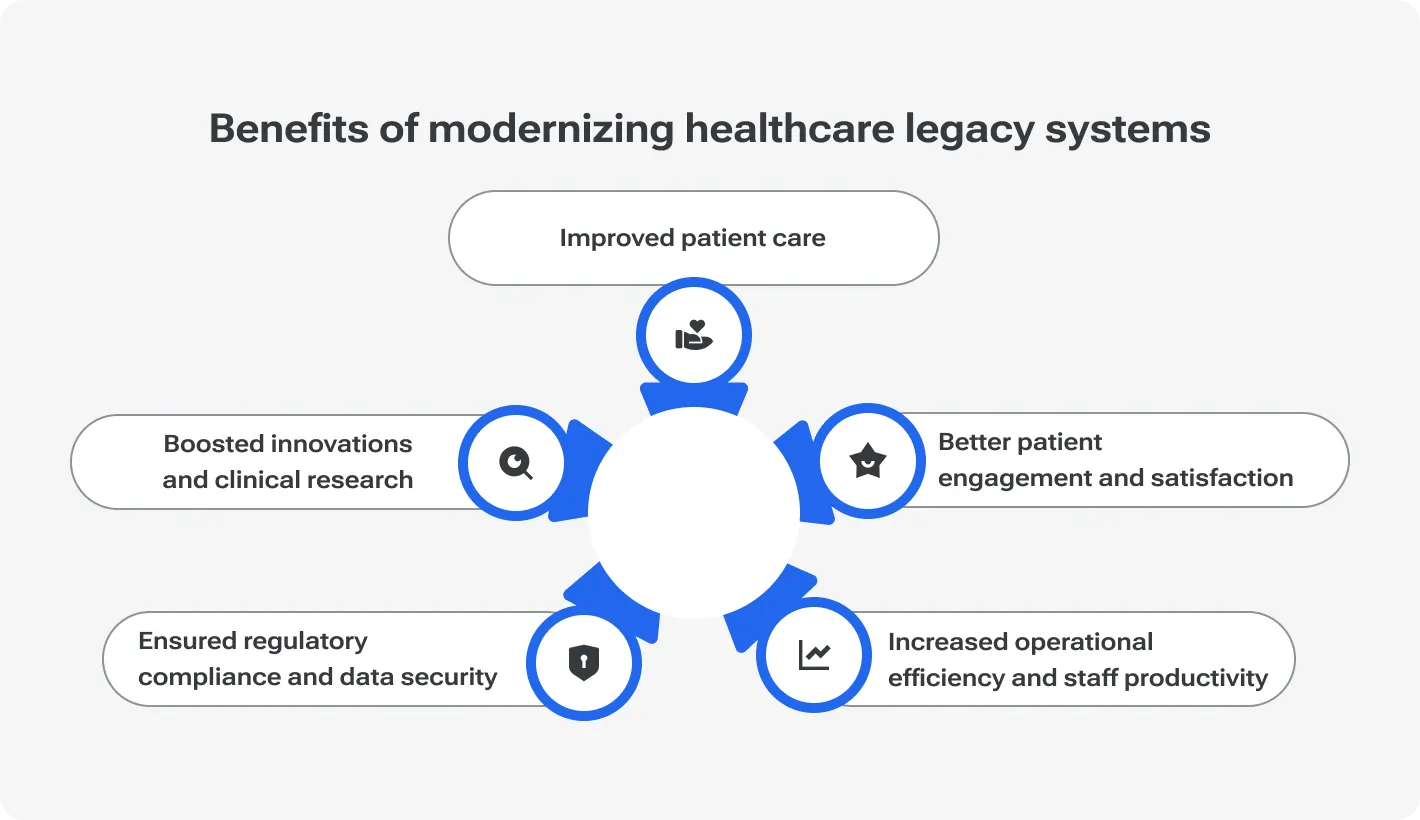
Benefits of Modernizing Healthcare Systems
Despite all these problems described above, most healthcare institutions still use outdated software. There are several reasons for this, like, the lack of strategic view and understanding of the importance of changes, or low IT qualification of the internal team, or deep integration of the legacy software with a system, or the lack of an urgent need to upgrade.
So, let's explore what would they get if they finally decided to update healthcare legacy systems.
Improved Patient Care
Modern systems give healthcare providers real-time access to complete patient data, including medical history, test results, and treatment plans. This allows them to make more informed decisions and provide personalized assistance.
Through seamless communication and information sharing between different departments and healthcare facilities, coordination of care and continuity for patients is significantly improved.
The latest clinical decision support tools, predictive analytics, and evidence-based recommendations will help healthcare specialists make accurate diagnoses and treatment decisions, hence, improving patient outcomes.
Better Patient Engagement And Satisfaction
Providing patient-centered medical care is not exactly a new approach, but it is the latest technologies that make it real and effective. Patients are engaged through dedicated patient portals, mobile apps, and telemedicine platforms. It allows them to take an active role in managing their health care, access health information and communicate with their doctors.
The latest developments help to create secure channels of communication between patients and healthcare providers, improving overall cooperation. It will also help to timely remind them about the appointment, and inform them about medications and instructions for further care. All of this ultimately improves patient satisfaction and adherence to treatment plans.
Increased Operational Efficiency And Staff Productivity
Automating routine administrative tasks, digitizing paper processes, and optimizing workflow management reduce manual errors and eliminate redundancies. All this increases the overall efficiency.
The correct allocation of resources is extremely crucial for today's medicine. Thanks to the latest technologies, the organization gets the opportunity to correctly assess the flow of patients and staff workload, use the available resources wisely, and predict the necessary transfers and replenishments. This allows healthcare organizations to optimize the use of resources, minimize wait times, and increase patient satisfaction.
Financial issues will also be resolved much faster. Streamlining billing and encrypting processes will reduce claim denials and accelerate reimbursement cycles. In this way, an increase in profit and financial efficiency of medical service providers is achieved.
Ensured Regulatory Compliance And Data Security
Compliance with data privacy regulations such as HIPAA and GDPR is one of the top requirements for healthcare organizations. Updated and state-of-the-art systems include robust security features, encryption protocols, and access controls that help to protect patient data from unauthorized access, hacking, and cyber threats.
Built-in analytics tools allow you to constantly check and keep documentation and processes in compliance with regulatory requirements. Most commonly it is used for electronic health record (EHR) interoperability standards, quality reporting initiatives, and billing regulations. This helps reduce the risk of fines and audits for non-compliance.
Last, but not least, healthcare legacy systems modernization boosts innovations and clinical research. It might be true not for all healthcare providers but for those, who strive to achieve progress in clinical trials and develop new treatments and therapies it is crucial. This is achieved due to the improvement of the ability to analyze large volumes of data, the rapid exchange of information between medical institutions, and the ability to constantly compare results in a short time.
Now, it is quite obvious that the benefits outweigh any disadvantages of the outdated systems.
Challenges in Modernizing Legacy Systems
Clearly, updating complex systems cannot be so simple, that it can be done in one or two months. In addition, several unforeseen obstacles may be encountered on the way, which will have to be solved urgently and by spending a lot of budget and time. So, what challenges can you face when updating your outdated healthcare systems?
Technical Issues: Outdated Technology Stack And Architecture
This is not always the case, but mostly outdated technology is the number one cause of most problems in legacy healthcare systems. The lack of necessary updates makes them limited and inflexible. The other side of the coin is that it is extremely difficult and expensive to maintain such systems, because there are fewer and fewer specialists who can still work with outdated technologies, and the new generation of IT engineers may not understand the specifics of the software and instead of making corrections, make even more mistakes.
Moreover, the complex multi-level architecture of such applications and programs does not allow updating at least part of the options in a short period and making necessary changes. The simplest solution offered is containerization, that is, fragmentation into microservices, and the transition to cloud storage to increase scalability and flexibility.
Integration Complexities With Existing Systems And Third-Party Solutions
Constantly growing demand and needs of patients require the introduction of the latest technologies and options. Which is almost impossible to do using outdated software. This also limits integration with other programs and organizations in the healthcare system, such as independent laboratories and research centers, which may use a different image or documentation format. Or restricts the integration of financial solutions that could significantly improve service delivery and patient satisfaction.
In matters of interoperability, standardized protocols adopted for a large number of medical institutions come to the rescue. Compliance with these standards requires updating the software, and in some cases, its complete replacement with newer systems. Currently, there are interoperability frameworks that can solve most of the problems, but their integration should take place only with the involvement of experienced specialists.
Data Migration And Conversion Issues
Storing large amounts of medical data about patients is the Achilles heel of most medical institutions. This requires high operating costs and constant resources for server maintenance and specialists. In addition, it makes exchange between departments of even one organization extremely difficult, let alone exchange between health care institutions.
The choice in favor of cloud storage has become one of the most widespread in recent years because it allows not only to efficiently store data but also to quickly get access to it. The main danger lies precisely in data migration and preserving their integrity. Before carrying out the migration, it is necessary to carefully check the data, remove duplicates, correct errors when they are detected, and make a backup version in case of data loss. A reliable cloud storage vendor will help with data migration and ensure its accuracy, completeness, and consistency.
Budget Constraints And Resource Allocation
In addition to the fact that updating outdated healthcare systems takes a long time, it is also very expensive. You will have to invest in upgrades for years and the costs can only increase over time. Of course, in this case, the question of the effectiveness of such changes arises. Nevertheless, you will be able to truly appreciate the financial benefit only after completing all the upgrade cycles.
However, you can control the budget and at least avoid overspending if you prepare a detailed upgrade plan and conduct a preliminary audit of the necessary changes. You should also turn to a trusted IT team if your internal resources are insufficient. Even if your engineers are highly qualified, they may not have time to work on several projects simultaneously, timely reinforcement by external programmers will make the work easier. Also, in some cases, you may need to prioritize upgrade tasks to optimize spending.
Regulatory Compliance And Privacy Concerns
Trying to achieve the best result It is also necessary to remember compliance with strict regulatory requirements such as HIPAA, GDPR, and interoperability standards when modernizing legacy systems. Taking into account these requirements can significantly complicate or slow down the process of updating data, yet, they cannot be ignored. Moreover, the security of patient data still remains a concern for most organizations.
It is not only about their integrity and storage method but also about ensuring protection and decent encryption against cyber-attacks and thieves trying to access the personal data of patients. This means that you should incorporate additional security protocols, and firewalls and strengthen protection systems when updating legacy healthcare software.
Another issue that you should keep in mind when planning to update legacy software is training your staff. After the update and the launch of the newest features, they will be the ones who will serve the patients and they must fully understand the new software to be as effective as possible in their places.
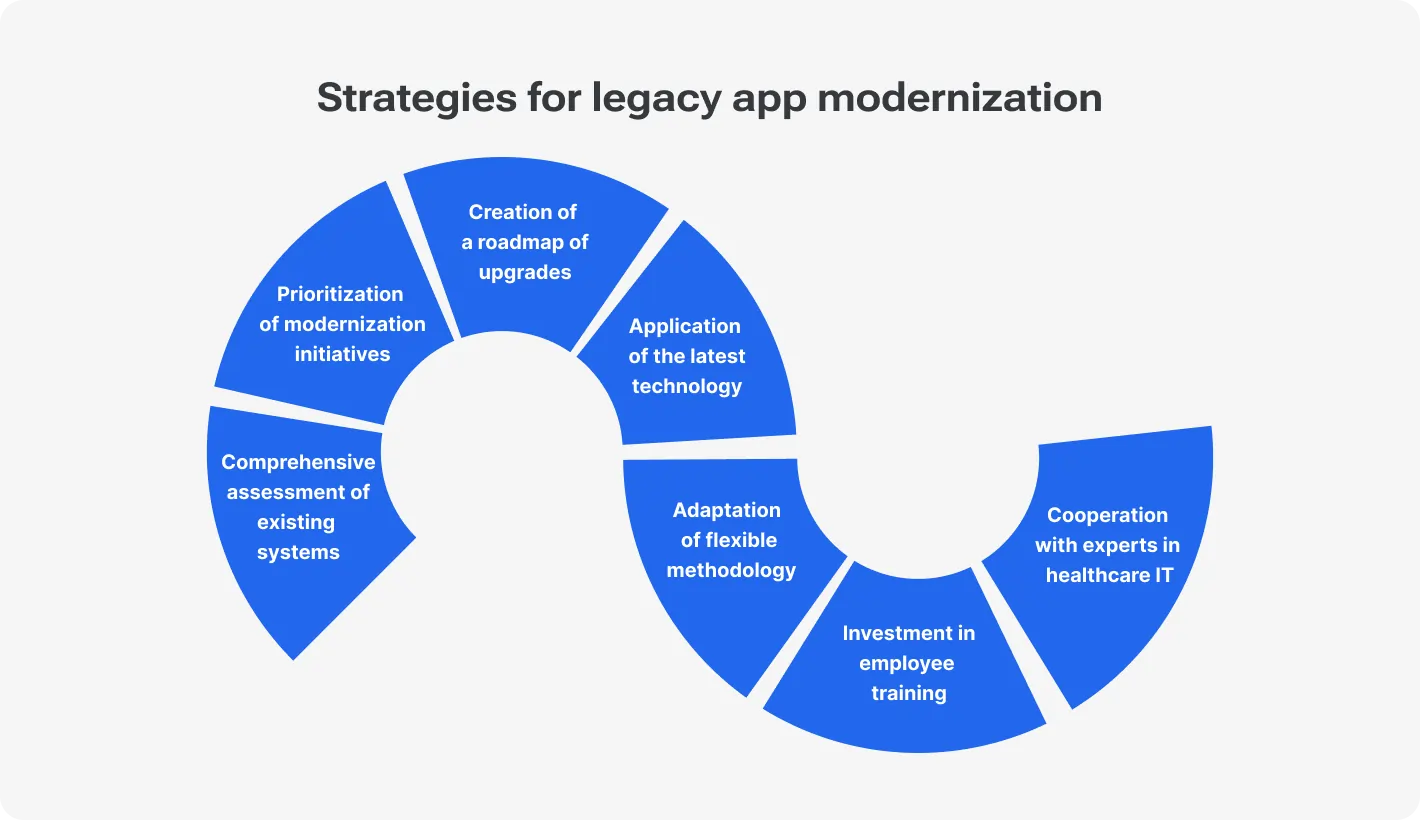
Strategies for Legacy App Modernization
Developing reliable legacy healthcare solutions it is recommended to start with a solid plan and here is a step-by-step algorithm you can follow at the very beginning.
Check existing infrastructure for readiness for an upgrade, test software and network infrastructure, and take a closer look at the technology stack, architecture, performance, security, and compliance. Look for areas of modernization, such as reducing technical debt and the risks of owning and maintaining legacy systems.
Focus modernization efforts on those objectives you wish to achieve with new systems, such as greater patient care and operational efficiency. Additionally, take the cost, regulatory requirements, system complexity, and impact on stakeholders into account.
Define modernization goals clearly and transparently, like transitioning to a cloud infrastructure, introducing new functionality, or improving security. Develop a concrete modernization roadmap with the priority, milestones, and scheduling of all modernization endeavors. Share the modernization plan with all stakeholders to gain coordination.
Find out how disruptive technologies like cloud processing, AI, ML, and IoT can modernize your legacy healthcare system. Deploy cloud storage, which is more scalable, adaptable, and cheaper than local servers. Explore opportunities to improve functionality and decision-making with AI and ML algorithms, or the potential of IoT devices and wearables for remote patient monitoring and telemedicine.
Save time and money with agile methodologies such as Scrum or Kanban. They are widely used to ensure iterative development and deployment of modernized solutions. Divide the roadmap into smaller, manageable sprints to focus on delivering specific features or improvements.
Ensure training for IT staff and other employees to familiarize them with new technologies, tools, and processes. Show employees and stakeholders the modernization benefits, highlighting how it will improve their workflows, productivity, and overall job satisfaction.
Reliable partners are crucial for successful legacy healthcare systems modernization. Collaborate with engineers specializing in healthcare IT to leverage their expertise and best practices. Build strategic partnerships with IT companies to co-create innovative solutions and address specific challenges.
Just a reminder: despite the rather detailed description, this is still an approximate list of steps and actions that you need to take when updating healthcare software. Each case may require additional steps or things to take into account.
Best Practices for Successful Legacy Software Modernization
Let's be honest. It is almost impossible to complete sophisticated tasks and avoid mistakes. Any path involves encountering possible weak points and obstacles that slow down, complicate, and in some cases, make it impossible to continue the way. In addition to using ready-made solutions of companies that have already gone through this path, you can also adopt best practices that will help minimize risks and avoid potential failures.
Engaging Stakeholders Across The Organization
One of the keys to successful modernization is transparent, reliable, and regular communication with all stakeholders throughout the process. Involve employees from various departments and levels of the organization in the modernization process to ensure diverse perspectives. Stay in touch with them to understand their workflows, pain points, and requirements.
Your IT staff should stay on the same page with all of them to apply their expertise in technology selection and implementation. If you work with an outsourced team, provide them with all necessary information and ensure regular updates.
Ensuring Alignment With Organizational Goals And Strategic Priorities
Always align modernization efforts with executives on all levels and strategic objectives to get necessary resources and support. The path of modernization is long enough to forget why it is all being done or get distracted by other tasks somewhere in the middle. Always keep the organization's goals, mission and strategic priorities in mind.
Prioritize modernization projects that have the greatest impact on achieving strategic goals, like improving patient care and operational efficiency, or reducing costs. Continually re-evaluate the alignment of modernization efforts with changing organizational priorities.
Communicating Transparently With Staff And Patients
Keeping in touch with staff and patients about the need for modernization, the goals of the initiative, and the expected benefits may save you tons of time on unnecessary explanations. Pick a reliable and suitable communication channel to inform them about changes made and expected in the future.
Provide regular updates and opportunities for feedback to address concerns. Educate staff and patients about changes in workflows, procedures and systems to ensure smooth adoption. Make short educational videos or brochures to provide them with all the necessary information.
Implementing Robust Security Measures To Protect Patient Data And Comply With Regulations
A solid security system is a must. Just develop a mix of special measures and incorporate them during modernization. You should prioritize data security and privacy at every step of the modernization process from design and development to implementation and maintenance.
HIMSS Healthcare Cybersecurity Survey highlights that in 2023 cybersecurity budgets are improving: 55.31% of respondents indicated that their budgets increased compared to the previous period, while 23.46% of respondents admitted their budgets stayed the same.
Implement encryption, access controls, authentication mechanisms, and intrusion detection systems to safeguard patient data against unauthorized access and cyber threats. Ensure compliance with regulatory requirements such as HIPAA, GDPR, HITECH Act, and industry-specific standards.
Monitoring And Evaluating The Impact of Modernization Efforts On Key Performance Metrics
Upgrading your legacy healthcare software, don't forget to evaluate the efficiency of the process. Define key performance indicators (KPIs) and metrics to measure the success and impact of modernization, for instance, patient satisfaction, operational efficiency, and financial performance.
Establish baseline metrics before modernization to track progress and assess the effectiveness of modernization initiatives over time.
Regularly monitor and evaluate performance metrics, get feedback from stakeholders, and adjust modernization strategies and priorities if needed to achieve desired results.
The main advice in all this is not to use all the best practices at once, choose those that will be organically carried out in your modernization process and that will be the most effective in your case. You can also develop your own methods and rules that will strengthen your project.
Real-Life Case Studies
From theory to practice. Industry leaders have been incorporating the latest technologies to update and modernize legacy software for many years now. They understand the importance and necessity of providing the highest quality healthcare services to patients like no one else. Let's dig into some of the most successful examples.
Kaiser Permanente Multi-Year Modernization Initiative
Kaiser Permanente, one of the largest integrated healthcare systems in the United States, faced lots of challenges with its legacy infrastructure: disparate systems, manual processes, and data silos.
They laid on a multi-year modernization initiative to standardize and integrate its systems, migrate to cloud-based platforms, and implement advanced analytics and digital health solutions.
"We are leveraging cloud appropriately and moving our architecture toward microservices and APIs to gain access to the data that is in our legacy systems," said Dick Daniels, executive vice president and CIO of Kaiser Permanente.
Kaiser Permanente also wagers on security and safety: "We are in healthcare, where security is a big concern. We are fortifying our infrastructure to protect against a constant barrage of security threats. At the same time, the organization is becoming more dependent on technology, so it is important that the technology be reliable, resilient, and robust."
Through the years, Kaiser Permanente improved care delivery, patient engagement, and population health management. The organization achieved better clinical outcomes, reduced hospital readmissions, and enhanced patient satisfaction through seamless access to care and personalized health services.
Geisinger Health System Legacy Modernization
Geisinger Health System, a regional healthcare provider in Pennsylvania, had issues with its legacy clinical documentation system. It was inefficient, error-prone, and lacked interoperability.
Starting with small yet crucial changes, Geisinger upgraded the old disjointed solution, which lacked options for clients' virtual interaction and appointment management. They've integrated it with necessary modules and functions which allow it to increase data accuracy, implement reliable appointment bookings and scheduling systems, and add virtual interactions with clients.
Following the industry trends, the organization modernized its clinical documentation system by implementing a cloud-based platform and AI to automate documentation, improve accuracy, and support clinical decision-making.
Geisinger Health System reduced documentation time for providers, improved data quality and completeness, and enhanced the patient experience. The organization also achieved better compliance with regulatory requirements and improved revenue cycle management through more accurate coding and billing.
The healthcare industry is constantly changing because it has to meet the demands and ever-growing needs of its patients. This means not only incorporating the latest treatment methods but also ways of interacting with patients and engaging them in the healthcare process. Legacy modernization opens new capabilities for industry leaders.
Wrap it Up
Legacy healthcare systems are among the main obstacles to the introduction of new technologies and options that could significantly improve patient care services. Moreover, the use of outdated software leads to delays in diagnosis, false conclusions and incorrect treatment.
Therefore, the modernization of legacy healthcare systems should solve the current issues and create the prerequisites for further scaling up taking into account the ever-growing needs and demands of patients. Undoubtedly, this is a long and complex process that requires significant investments of time and budget. However, in the end, you get the opportunity to achieve business goals with a patient-centric approach. Your profits depend on patients' satisfaction, whether you improve performance or implement new options.
A few quick tips: don't rush to update everything, focus on urgently needed changes; create an upgrade plan in advance, according to the structure and complexity of your system; constantly evaluate the effectiveness of changes and adapt the most flexible way of making them; communicate with all stakeholders to understand in time whether you are meeting their needs. In addition, don't hesitate to find a professional IT healthcare team specializing in legacy modernization for complex projects.
Transform your legacy systems to boost efficiency and innovation